The body is a complex, impressive assembly of millions of parts. Yet, a body is just that – one body, a singular structure.
The body’s parts are designed to work together. Thus, when a problem arises in one area, it tends to affect other areas. For instance, a slipped or herniated spinal disc can trigger painful sensations that run from the back, hip and down one or both legs.
One of the reasons I undertook advanced training in neuromuscular dentistry was because of the far reaching associations involving the alignment of teeth; size of the tongue; shape of the palate; connecting muscles and tissues; and associated joints.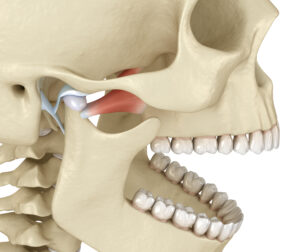
An area of particular concern in neuromuscular dentistry has to do with the temporomandibular joints (TMJ). These joints, located on the sides of the head, connect the lower jaw to the temporal bones. These joints allow the lower jaw to glide up and down and side to side, enabling movements for speaking, biting and chewing.
What’s in control of the position and movements of the joints are the muscles attached to them. When we open our mouths, the rounded ends of the lower jaw, (condyles) rotate within the joint sockets. Like most bones in the body, the condyles rely on a disc between it and the temporal bone to keep the movement fluid and absorb shock.
Yet, like discs in the spinal column that cause pain to shoot down a leg, improper bite alignment can cause problems that extend to far reaching locations, some that may seem to be unrelated to a misaligned jaw joint.
Typically, misalignment of teeth is the source of TMJ disorders. The stress or strain transferred from an incongruent position of teeth leads to wear and tear on the jaw joints. This results in inflammation that activates problems in areas associated with these joints. However, research is finding the connection of the jaw joints to other conditions can reach much further, in many cases.
As a neuromuscular dentist, I find the complexity of TMJ disorder is being looked at far more as research brings to light it as the source of a number of problems. Some of those traditionally associated with the TMJ are:
• Jaw soreness, especially upon awakening
• Frequent headaches or migraines
• Pain in the face, shoulder, neck, or behind the eyes
• Earaches or ringing in ears
• Jaw clicking or popping
• Difficulty opening the mouth fully
• Clenching or grinding of teeth during sleep
• Dizziness
• Sensitive teeth
• Numbness or tingling in the fingers
• Shifting or loosening of teeth
According to a publication of TMJ.org:
Recent research results have demonstrated that TMJ disorders are complex medical conditions that involve multiple body systems, rather than just a localized jaw condition. The cardiovascular, neurological, immunological, digestive, respiratory, endocrine and musculoskeletal systems contribute to the onset, development and/or persistence of TMJ, as well as influence treatment outcomes.
Thus, the association of health problems connected to the TMJ is coming to light. And none too soon. The numbers have nearly doubled from those pre-Covid.
The National Institutes of Health shares, in a report following the pandemic:
“The rate of TMDs (worsening of previous TMDs or new onset) during the COVID-19 infection period among participants was 41.9%.”
Disorders of the jaw joint and chewing muscles can vary widely. Some people have other health problems that co-exist with TMJ disorders. These may include chronic fatigue syndrome, sleep disturbances or fibromyalgia. Because these health problems share certain symptoms, it is suspected they could also share similar disease activation factors. 
And, this can be a back-&-forth problem, which is to say that TMJ disorders (TMD) could be triggering other disorders, or that other disorders may be contributing to TMD. For example, conditions that affect other joints in the body, as in arthritis, may cause or aggravate TMJ disorder. Some of the health issues that may contribute to the disease are:
– Sinusitis
– Sjogren’s syndrome
– Sleep disorders
– Psychological symptoms (such as depression, anxiety and post-traumatic stress disorder)
– Systemic lupus erythematosus
– Tinnitus
– Vertigo
Diagnosing TMD as a contributing factor related to the above is often lost due to lack of awareness and training in the relationship between the two. Misdiagnosis is common when clinicians are unaware of the correlation between these conditions. That is starting to change as more research shows the undisputed connections.
Scientists have found that 85% of patients with TMJ disorder also suffer from both chronic pain and non-pain conditions in other parts of the body. For example, studies have shown that the following health conditions have a greater likelihood of coexisting with TMJ disorders, particularly in females (listed in the 2020 National Academy of Medicine report on TMJ):
• Ankylosing spondylitis in other body joints
• Asthma
• Back, neck, and joint pain
• Chronic fatigue syndrome
• Endometriosis
• Fibromyalgia
• Irritable bowel syndrome (IBS)
• Headaches
• Heart disease
• Hypertension
• Interstitial cystitis/painful bladder syndrome
• Juvenile idiopathic arthritis in other body joints
• Neural/sensory conditions
• Osteoarthritis
• Poor nutrition due to alerted jaw function and/or pain while chewing
• Psoriatic arthritis
• Respiratory conditions (e.g., sinus trouble, allergies or hives, asthma, tuberculosis, breathing difficulties)
• Rheumatoid arthritis
How is TMJ disorder correctly diagnosed?
In addition to having advanced neuromuscular dental skills, our Shelby Twp dental office features highly-advanced, computerized imaging technology that reveals the very source of pain resulting from TMJ issues. In some findings, the TMJ is not the true source of the problem. However, if it is, this technology shows us where it is and why it occurs.
The TMJ diagnostic process is painless and much faster than outdated, “best guess” methods often used in dental offices. For example, we use: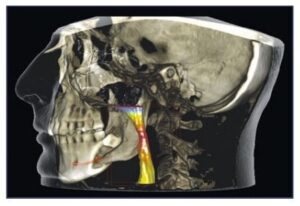
CONE BEAM 3D imaging for intricate, concise views far and beyond what a typical ‘bite wing’ or Panorex (jaw to jaw) affords. In a single scan, these 3D images show teeth, soft tissues, nerve pathways and bone. For TMJ patients, these images are ideal for assessing the position of the jaws, evaluation of the jaw joints, and review of airway passages.
BIOPAK system records the functions and congruity of the upper and lower jaw, jaw joints, and associated muscles at various ranges. This aids in proper diagnosis and treatment planning for TMJ dysfunction, sleep disorders and head/facial pain – with results available the same day.
TEKSCAN (T-Scan™) Digital Occlusal Analysis is the only technology that shows the measured force and the timing of occlusal surfaces coming together, providing a clear picture of the patient’s bite.
If you suspect you are clenching or grinding at night or have sore jaw joints, facial pain, frequent headaches or other symptoms as listed above, consider a no-charge consultation appointment in our comfortable, modern dental office. We provide complete dentistry for all needs, including cosmetic dentistry and all stages of dental implants and are always pleased to welcome new patients!
Call 586-739-2155 or tap here to begin. You are also invited to watch a brief video on TMJ disorder care in our office: DrBarbatTMJ
And, enjoy a quick tour of our Macomb County dental office at: DrBarbatOfficeTour
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9491629/
https://nap.nationalacademies.org/read/25652/chapter/1#iii
https://tmj.org/living-with-tmj/diagnosis-and-related-conditions/related-conditions/
https://www.ucsfhealth.org/conditions/temporomandibular-joint-disorders
https://tmj.org/living-with-tmj/diagnosis-and-related-conditions/related-conditions/